Malignant Fibrous Histiocytoma (MFH; Undifferentiated Pleomorphic Sarcoma UPS)
GENERAL INFORMATION
Malignant Fibrous Histiocytoma was first described in the 1960s presumably derived from a mixed histiocytic and fibroblastic cellular origin but is it now believed that it is a lesion derived from fibroblast differentiation. It is a malignant neoplasm (sarcoma) of mesenchymal/spindle origin. It is a high gade sarcoma with a strong potential for metastatic disease. Since the beginning MFH was recognized as a heterogeneous group of tumors with varying histology affecting both genders and all ages. Since 1978, MFH it was identified as the most common soft tissue sarcoma after Weiss and Enzinger published the first large series of tumors with those characteristics.
Four different sub-types have been described: Storiform-pleomorphic, Myxoid, Giant cell and Inflammatory. It is now often referred to as Undifferentiated Pleomorphic Sarcoma (UPS).
Of these, the storiform-pleomorphic is the most common type, accounting for up to 70% of the cases. The myxoid variant is the second most common accounting for approximately 20% of cases. After 2002 The World health Organization suggested replacing the term MFH with Undifferentited high-grade pleomorphic sarcoma (UPS). Myxoid MFH is now myxofibrosarcoma. Giant cell MFH and inflammatory MFH are now called UPS with giant cells and UPS pleomorphic sarcoma with prominent inflammation, respectively.
CLINICAL DATA
Comprises 20% - 30% of soft tissue sarcomas
Second most common type of soft tissue sarcoma
Most commonly arises from the soft tissues but may arise from bone.
Most common soft-tissue sarcoma in adults though it can appear at any age. Very rare in patients < 20 year old.
Most common sarcoma after radiation.
Heterogeneous tumor in histology and prognosis
Early osseous invasion and metastases to regional lymph nodes may occur
CLINICAL PRESENTATION
Signs/Symptoms
Rapidly enlarging, painless mass. 30% of patients may have dull aching pain or tenderness.
Some patients report trauma in the affected area (trauma does not cause MFH) and the MFH may be misconstrued as a hematoma or muscle strain
Systemic symptoms are not expected.
Prevalence
Male predilection (70%)
More frequent in caucasion population
Age
Most cases occur between 50 and 70 years old.
Extremely rear in children.
Sites
Lower extremity
50%
Most commonly arises in the thigh
Upper Extremity
25%
Retroperitoneum
15%
Head/neck
5%
RADIOGRAPHIC PRESENTATION
Deep intramuscular soft mass
Average size of 5 to 10 cms.
Heterogeneous mass
Osseous involvement is frequent
Regions of mineralization may be demonstrated on plain x-rays but is unusual for an MFH
In some cases, MFH can be more aggressive and invade an adjacent bone.
Plain x-ray
Demonstrate a soft tissue mass density.
Curvilinear or punctate mineralization may be observed in 5 to 20% of patients.
Heterotopic bone formation may rarely be present along the periphery of the mass.
It is not the ideal method of study in cases of MFH.
CT scan
Nonspecific, large, soft tissue mass of predominantly muscle density, with nodular and peripheral enhancement of solid portions.
Central areas of low attenuation reflecting necrosis, hemorrhage or myxoid regions.
Fat attenuation is not observed.
MRI (Fig. 1-5)
Typically reveals an intramuscular mass with heterogeneous signal intensity reflecting variable amounts of collagen, myxoid tissue, necrosis, and hemorrhage.
Low to intermediate signal intensity on T1-weighted. (Fig. 1 Ax T1 SE1)
Intermediate to high signal on T2-weighted. (Fig. 4)
Viable areas enhance with contrast (Fig. 3)
Low intensity in T1-weighted and high density in T2- weighted reflecting high water content (Fig. 1, 2 &4)
Areas with prominent fibroid tissue demonstrate low density in T1 and T2 weighted images.
Regions of hemorrhage have high signal on T1 and T2 weighted images.
Necrosis have similar pattern as fluid (Fig. 5 SAG T1 FS postcontrast)
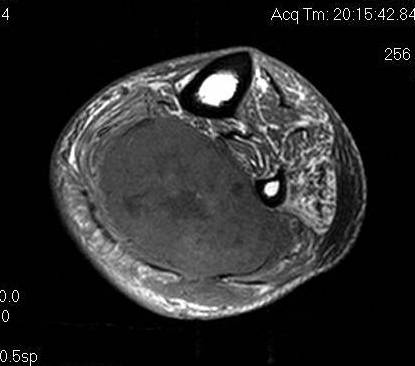 Fig. 1
Fig. 1
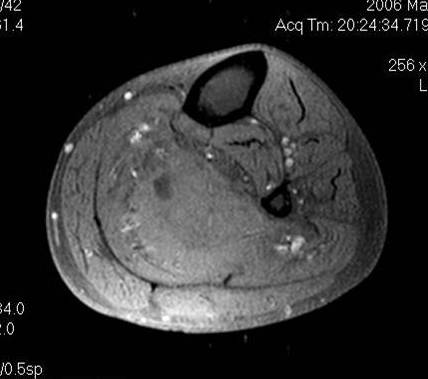 Fig. 2
Fig. 2
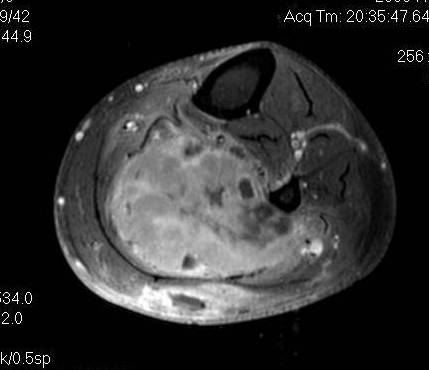 Fig. 3
Fig. 3
 Fig. 4
Fig. 4
Fig. 1, Fig. 2 & Fig. 4 T1W, T1W Fat suppressed and T2 W fat saturated MRI demonstrate a large calf mass (MFH) in an intramuscular location within the soleus muscle.
Fig. 3 T1W fat suppressed postcontrast MRI. Irregular peripheral, septal, and nodular enhancing elements in this malignant fibrous histiocytoma. Non enhancing areas correspond with necrosis and hemorrhage. The enhancing areas are those that should be biopsied.
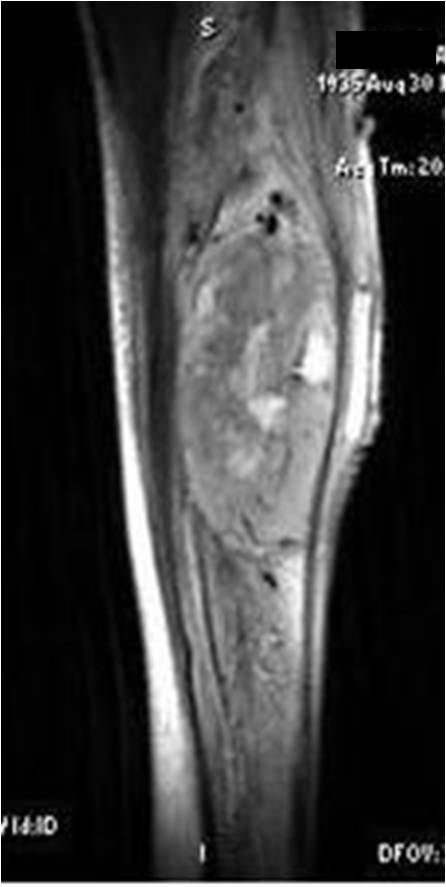 Fig. 5 Sag STIR MRI images of a malignant fibrous histiocytoma demonstrate a mass with heterogeneous signal intensity reflecting variable amounts of collagen, myxoid tissue, necrosis, and hemorrhage.
Fig. 5 Sag STIR MRI images of a malignant fibrous histiocytoma demonstrate a mass with heterogeneous signal intensity reflecting variable amounts of collagen, myxoid tissue, necrosis, and hemorrhage.
PATHOLOGY
Gross Pathology (Fig. 6)
Well circumscribed, expansile mass (pseudocapsule of compressed tissue around periphery gives circumscribed appearance)
Lobular growth pattern
Peripheral pseudocapsule
After cut surface; pale fibrous or fleshy areas mixed with areas of hemorrhages, necrosis or myxoid tissue.
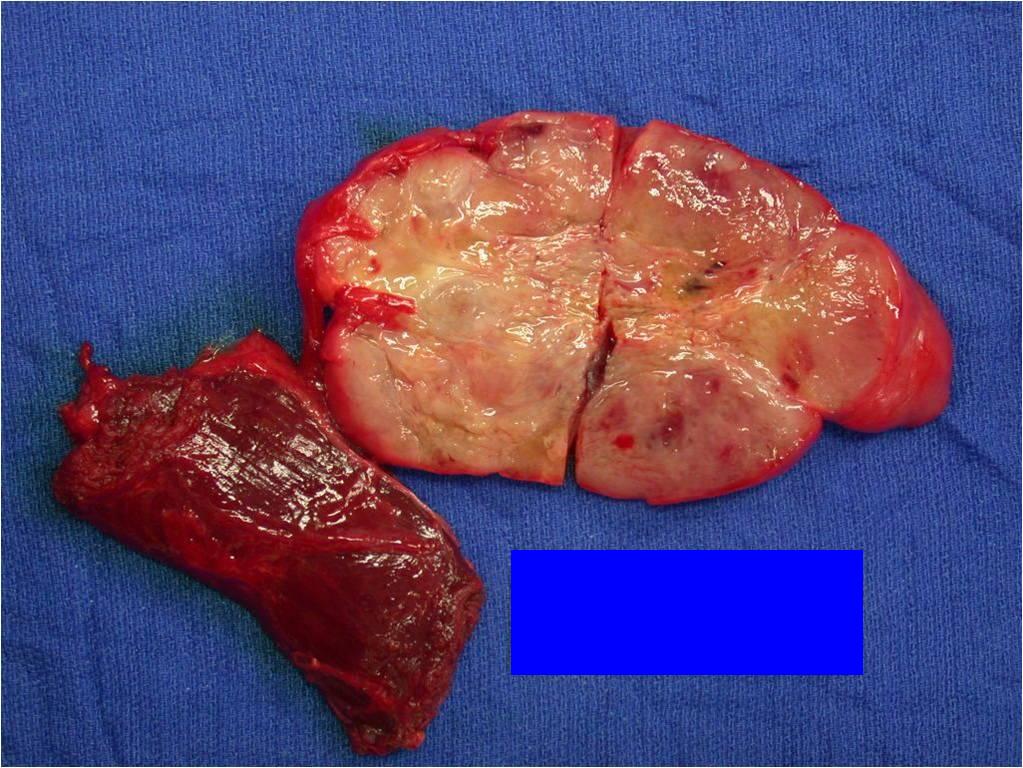 Fig. 6 Gross Pathology: Well circumscribed mass, multiloculated growth pattern. A thin peripheral pseudocapsule is present. Fleshy areas mixed with areas of hemorrhages and necrosis.
Microscopic Pathology (Fig. 7A, 7B &7C)
Fig. 6 Gross Pathology: Well circumscribed mass, multiloculated growth pattern. A thin peripheral pseudocapsule is present. Fleshy areas mixed with areas of hemorrhages and necrosis.
Microscopic Pathology (Fig. 7A, 7B &7C)
Anaplastic sarcoma composed of varying amounts of pleomorphic fibroblasts
Scant cytoplasm and significant nuclear pleomorphism with abundant atypical mitotic figures
Bizarre giant cells mixed with spindle cells, myofibroblast histiocyte-like cells and undifferentiated cells.
May have substantial myxoid components, inflammatory tissue and giant cell rich areas
Storiform pattern of arrangement of cells and matrix (swirling pattern of collagen bundles and cells)
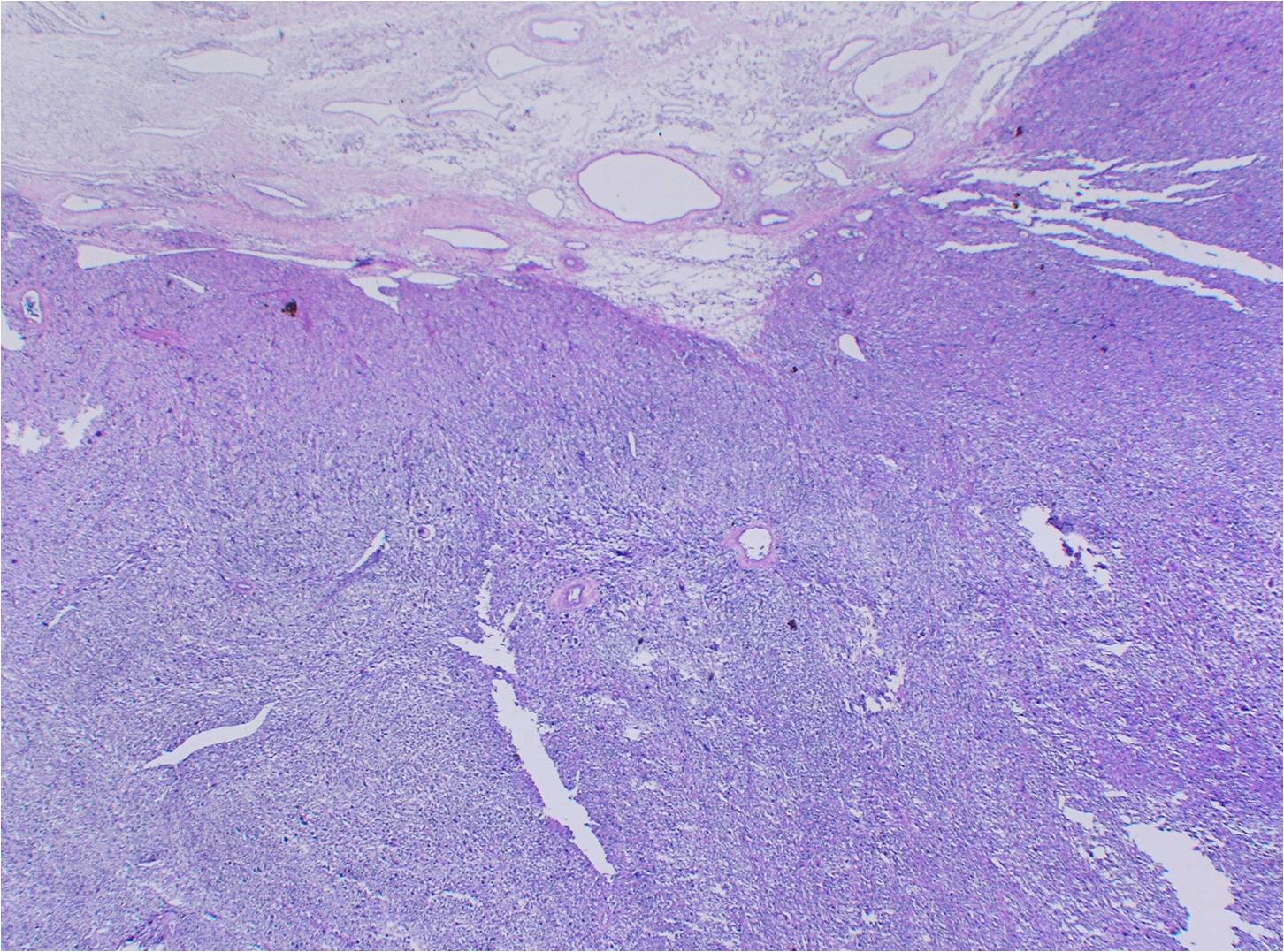 Fig. 7A
Fig. 7A
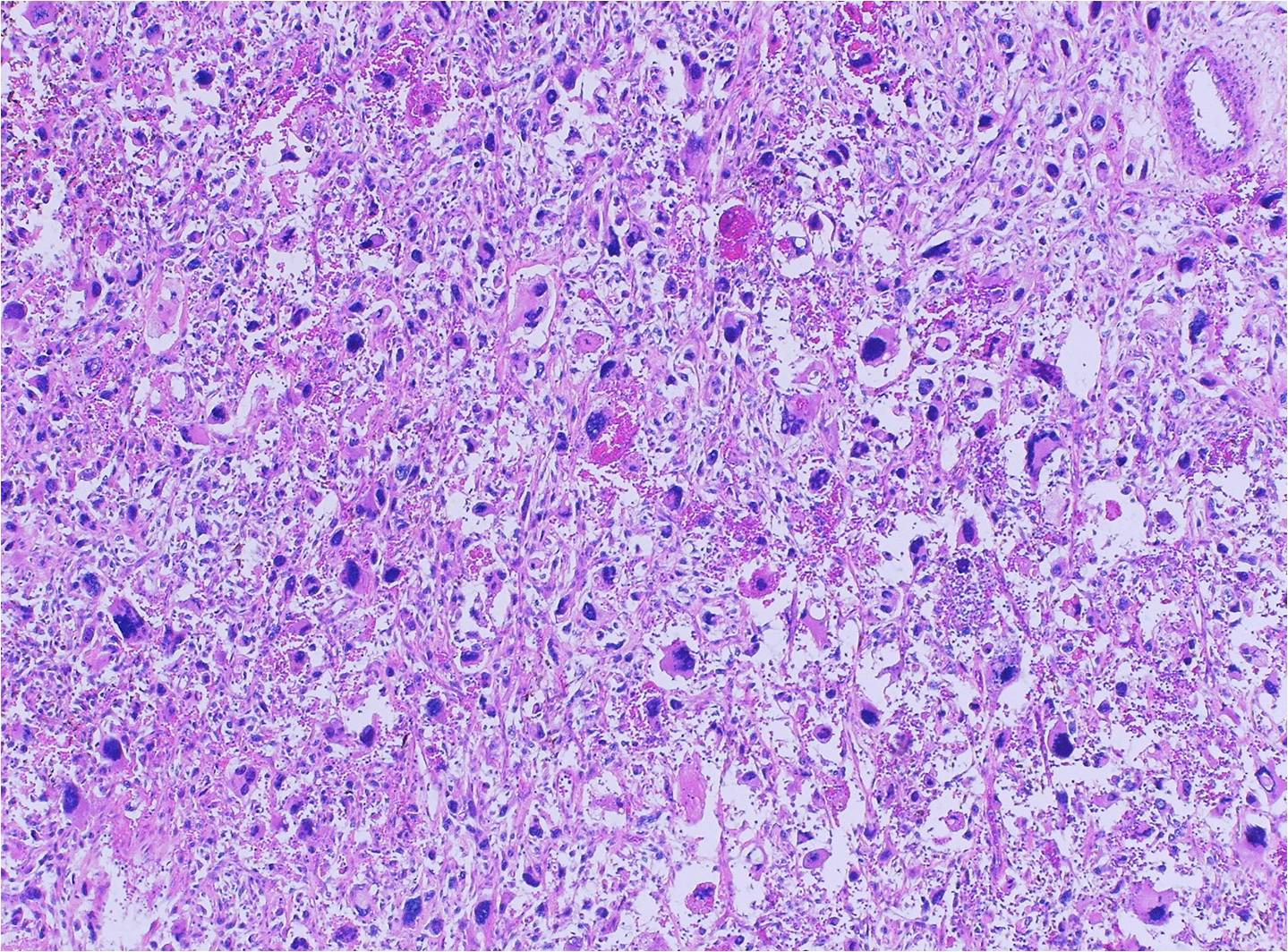 Fig. 7B
Fig. 7B
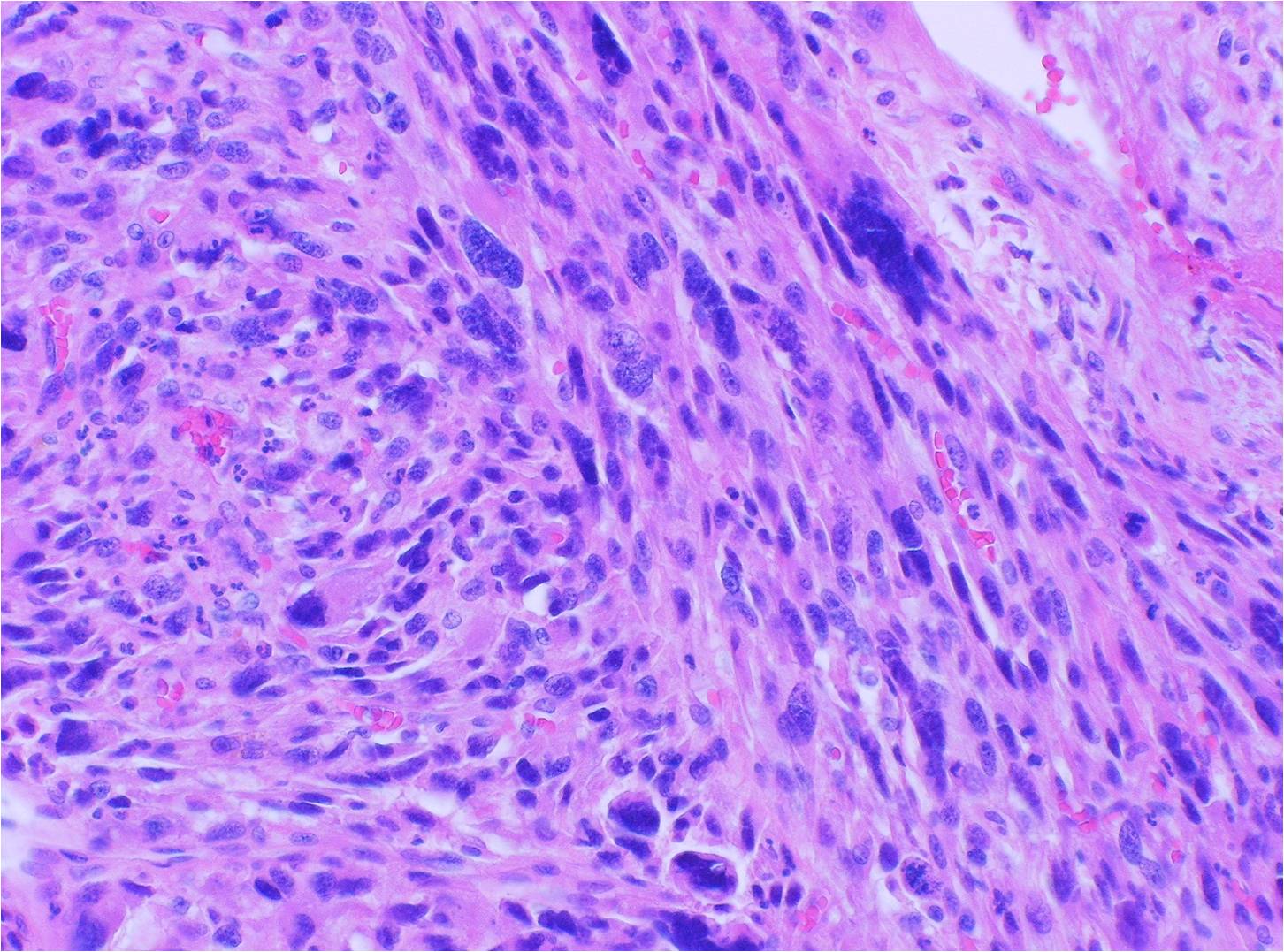 Fig. 7C
Fig. 7 Microscopic Pathology: Low (A), medium (B) and high magnification (C) E&H staining demonstrate a hypercellular spindle call neoplasm with large nuclei and scant cytoplasm as well as significant nuclear pleomorphism and abundant atypical mitotic figures. There are many bizarre appearing large cells. It is possible to identify multiple giant cells mixed with spindle cells. There is fibrous tissue admixed with the cells (fibrous stroma). The cells and fibrous tissue are arranged in a storiform or swirling arrangement.
Fig. 7C
Fig. 7 Microscopic Pathology: Low (A), medium (B) and high magnification (C) E&H staining demonstrate a hypercellular spindle call neoplasm with large nuclei and scant cytoplasm as well as significant nuclear pleomorphism and abundant atypical mitotic figures. There are many bizarre appearing large cells. It is possible to identify multiple giant cells mixed with spindle cells. There is fibrous tissue admixed with the cells (fibrous stroma). The cells and fibrous tissue are arranged in a storiform or swirling arrangement.
PROGNOSIS
Biological behavior
Metastases (35% to 45% of patients)
Lung (90%)
Bone (8%)
Liver (1%)
Lymph Nodes (1%)
Prognosis: 5 years survival overall 65%
TREATMENT
Wide surgical resection and postoperative radiation whenever feasible (Fig. 8)
Amputation for unresectable tumors.
Attention is directed to ruling out metastases to the regional lymph nodes
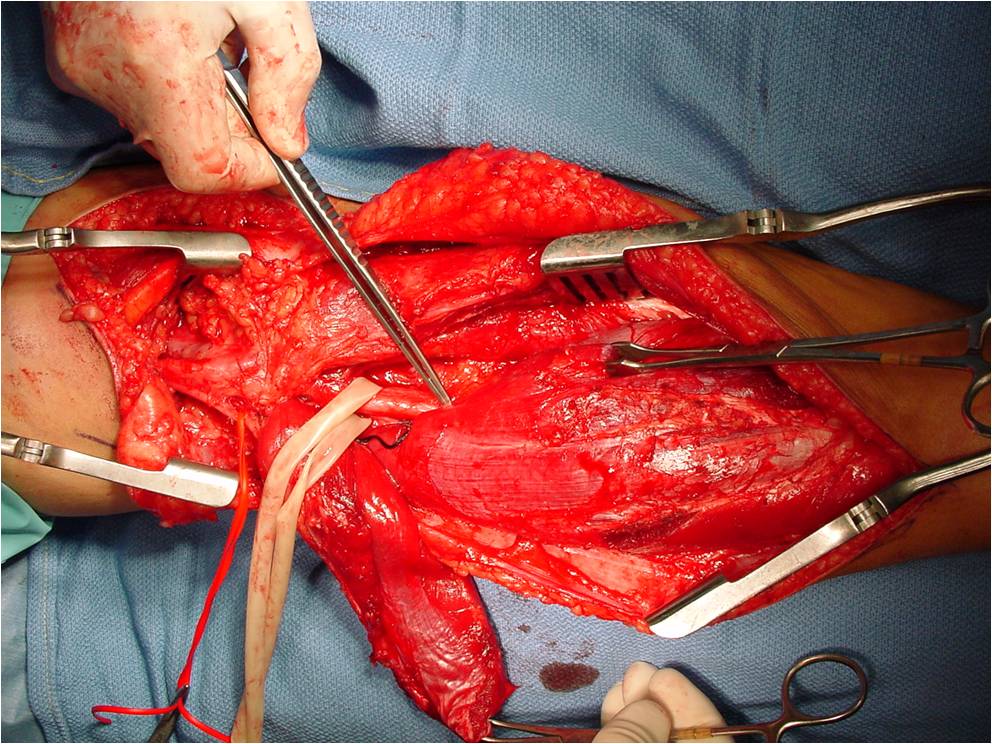
Fig. 8 Intraoperative image demonstrates a posterior approach to the calf for removal of a malignant fibrous histiocytoma. Neurovascular dissection and wide excision of the mass.
